back to main
page
 Chiari
Malformation
Chiari
Malformation
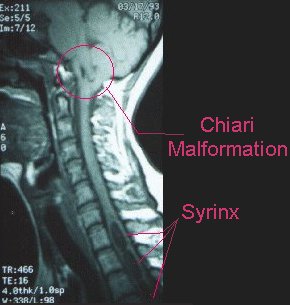
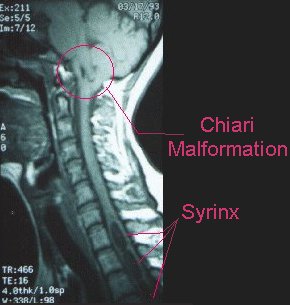
Also known as Arnold-Chiari Malformation or ACM, this is a very rare structural
condition affecting the cerebellum. Essentially there is extra cerebellum crowding
the outlet of the brainstem/spinal cord from the skull on its way to the spinal
canal. This crowding will commonly lead to severe headaches, neck pain, loss
of balance, tingling in the arms and/or legs, stiffness, and less often will
cause problems such as chronic coughing, difficulties with swallowing, and choking.
Often the symptoms are made worse with straining.
Untreated, the chronic crowding of the brainstem and spinal cord can lead to
very serious consequences including paralysis. In addition they can lead to
the development of syrinxes which may further injure the patients spinal cord
and function. These malformations are very difficult to see on CT scans and
impossible to see on plain x-rays.The Chiari Malformation can be seen in MRI's
showing the cranio-cervical junction (either brain or Cervical Spine MRI's).
Typically, radiologists only know the "traditional" definition of
Chiari, as tonsillar herniation. Also, many neurologists and neurosurgeons
haven't heard of chiari, while others have learned the "traditional"
definition of CM. All of these things contribute to the common
misdiagnosis of the condition.
Chiari can present with a wide variety of symptoms,
because the cerebellum and the brainstem are often compressed, which leads
to a variety of neurologic symptoms.
There are many ways to treat Chiari malformations, but all require surgery.
The basic operation is one of uncrowding the area at the base of the cerebellum
where it is pushing against the brainstem and spinal cord. This is done by removing
a portion of bone at the base of the skull deep to the neck muscles as well
as often removing a part of the back of the first and occasionally additional
spinal column segments.
After so much controversy
and confusion regarding chiari and it's diagnosis, this is a landmark
study by Dr. Thomas Milhorat, from the Chiari Institute. If all neurosurgeons
would read this, it would put an end to misdiagnosis and confusion. (Let
me know if you have any trouble viewing pdf (acrobat) files.)
Here are some other
sites that have good information about Chiari (some of the design/navigation
is better than others, but that can't be helped).
The
Chiari Institute (with overviews of Chiari Malformations, Syringomyelia,
diagnosis, treatment etc)
Overview
about Chiari
Chiari
Syringomyelia News
They also have some pdfs of patient awareness sheets and stuff you can download
and print out (Chiari
Awareness sheet, Syringomyelia
Awareness sheet, Chiari
Patient Education sheet, Syringomyelia
Patient Education sheet).
The
World Arnold Chiari Malformation Association Click the onsite info link
to start with...there is a lot there.
Chiari
Malformation I
American
Syringomyelia Alliance Project (ASAP)
Syrinx/Syringomyelia
(being looked at as a matter of course)(NOTE: This was ruled out for
me)
Syringomyelia, often referred to as SM, is a chronic disorder involving the
spinal cord. For reasons that are only now being understood, cerebrospinal fluid
enters the spinal cord, forming a cavity known as a syrinx. (Doctors sometimes
use other words such as cyst, hydromyelia or syringohydromyelia) This syrinx
often expands and elongates over time, destroying the center of the spinal cord.
As the nerve fibers inside the spinal cord are damaged, a wide variety of symptoms
can occur, depending upon the size and location of the syrinx. There are two
major types of SM. In most cases it is related to a congenital malformation
involving the hindbrain (cerebellum) called a Chiari I Malformation, named after
the physician who first described it. This malformation occurs during fetal
development and is characterized by downward displacement of the lower part
of the brain (cerebellar tonsils) beneath the foramen magnum, into the cervical
spinal canal. This displacement blocks the normal flow of cerebrospinal fluid.
When normal flow is obstructed, a syrinx can then form in the spinal cord. Not
all patients with Chiari Malformations will develop a syrinx, however.
SM can also occur as a complication of trauma, meningitis, tumor, arachnoiditis,
or a tethered spinal cord. In these cases the syrinx forms in the section of
the spinal cord damaged by these conditions. As more people are surviving spinal
cord injuries, more cases of post-traumatic SM are being diagnosed as the syrinx
can form years after the trauma.
Spina
Bifida Occulta (being looked at due to red markings on my lower
back and a coccygeal pit (dimple) also on my lower back)(NOTE: This
was ruled out for me)
Spina bifida is
a defined as any abnormal development of the bones of the spine that display
a typical pattern, with or without the involvement of the brain, nerves or covering
of the nerves (meninges). It is the most common congenital spine abnormality.
The term spina bifida covers a range of malformations that always include deformities
of certain parts of the vertebrae, the spinous process and vertebral arch. Some
have described this process as a failure of these bones to fuse during early
fetal development.
Most common locations are the lower thoracic, lumbar, and sacral spine. The
cause behind this congenital malformation is not well understood. Data suggests
that genetic factors play a predominant role, but nutritional and environmental
factors may also contribute to the development of spina bifida. Spina bifida
is broken down into two categories: spina bifida occulta and open spina bifida.
These subtypes are distinguished by the absence or presence of nerves, fluid
that surrounds the nerves (CSF), and the meninges that are included within the
deformity.
Since there is
no opening to the skin, spina bifida occulta can only be seen on x-ray or MRI.
Certain clinical findings such as dimpling of the skin or a hairy patch at the
base of the spine may trigger further investigation by a physician. Underlying
spinal nerve abnormalities can be seen in these situations. There is inconclusive
evidence that this type of deformity is related to back pain, scoliosis, or
nighttime bed-wetting. A large study showed that in patients not complaining
of back pain, almost 20% had uncomplicated spina bifida occulta. If you have
an abnormality on an x-ray, it does not always mean that this is causing your
pain.
A good site is the Spina Bifida Association of
America.
Tethered
Cord (being looked at due to red markings on my lower back and
a coccygeal pit (dimple) also on my lower back)(NOTE: This was ruled
out for me)
Tethered Spinal
Cord Syndrome is a disorder characterized by progressive neurological deterioration
that results from compression of the lowermost bundle of nerves of the spinal
cord (cauda equina). It is most commonly associated with a defective closing
of the neural tube (precursor of the spinal column) during embryonic development
(Spina Bifida).
The spinal cord extends from the base of the brain through the boney spine to
the lower back. Soon after conception, special cells come together to form a
tube that will become your baby's spinal cord. If this tube does not completely
close, the spinal cord can become tethered. The cord is said to be "tethered"
when it is abnormally attached within the boney spine.
The spinal cord can also become tethered with spina bifida occulta. This can
occur without visible outward signs although usually half the children have
visible symptoms.
This may not be a problem until the child develops symptoms. Normally the spinal
cord is able to move freely when your child bends or stretches but when it is
tethered, it is stretched, especially with those movements. This abnormal stretching
puts tension on the cord that can cause permanent damage to the muscles and
nerves that control the legs, feet, bowel and bladder. Early detection and treatment
is important to prevent this from occurring.
* Note the pic
on this page isn't of me, just an example image.
 Chiari
Malformation
Chiari
Malformation